
Diabetic retinopathy (DR) can lead to moderate to severe vision loss, and is the main cause of blindness in long-term diabetic patients. Typically, this disease does not show obvious symptoms before it develops to an advanced stage. Regular follow-up can detect and prevent up to 98% of visual loss caused by DR at an early stage.
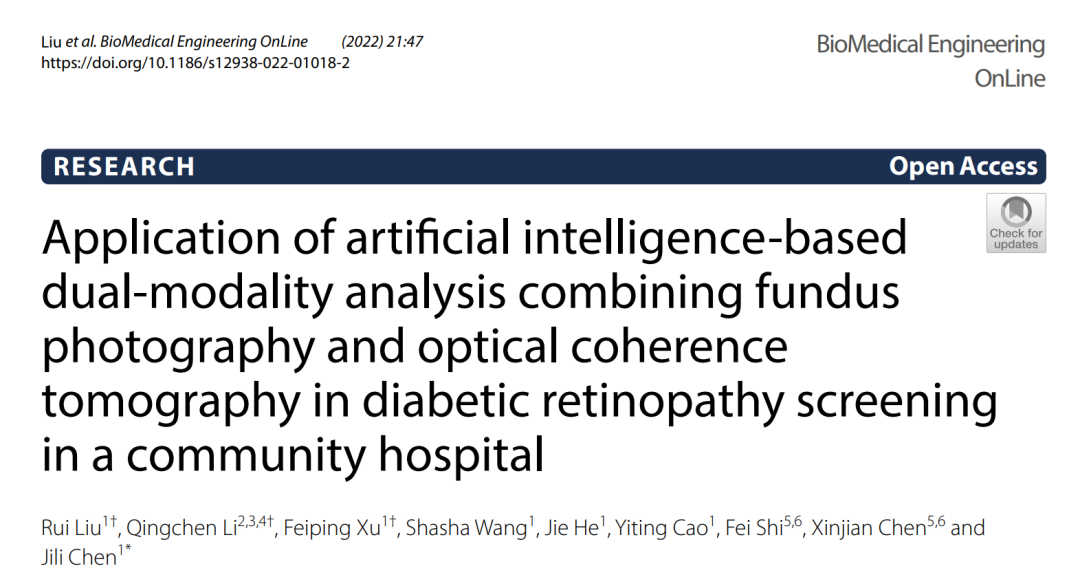
In recent years, artificial intelligence (AI) screening for DR based on fundus photographs has shown high accuracy, sensitivity and specificity. However, some defects have also been found in the screening process, especially in the identification of diabetic macular edema (DME). Since the diagnosis of DME requires the identification of macular thickening, using 2D fundus photos to screen for DME may lead to errors. Optical coherence tomography (OCT), as the main tool for detecting macular diseases, will further improve the sensitivity of detecting retinal diseases through screening tests.

Professor Chen Jili’s team from Shanghai City North Hospital, together with Suzhou Big Vision Medical Technology and Professor Chen Xinjian’s team from Suzhou University, conducted a study on the application of dual-modal AI based on fundus photography and OCT developed by Big Vision Medical in diabetic retinopathy (DR) screening in community hospitals. The results were recently published in Biomedical Engineering Online (IF3.903). This study confirmed that dual-modal AI screening can detect more cases of DR that require referral, and the consistency with expert reading results is relatively high. The application of fundus photography and OCT dual-modal AI-assisted diagnosis technology in the screening of diabetic retinopathy in the community is feasible.

read the original paper.
Abstract
Objective:
To evaluate the accuracy of a dual-modal AI algorithm combining fundus photography and OCT in DR screening, and to explore the feasibility and application value of this dual-modal screening mode in community hospital DR screening.
Methods and Discussion:
From October 2019 to December 2019, non-mydriatic fundus photography and optical coherence tomography (OCT) were performed on 600 diabetic patients who visited the community hospital outpatient clinic, including 324 males and 276 females. The mean age of the study subjects was 67.26±7.02 years. According to the International Clinical Diabetic Retinopathy (ICDR) severity scale, DR with moderate or higher degree or the presence of ME was defined as referable diabetic retinopathy (RDR). All fundus photographs and OCT images were independently recognized and classified by the Big Vision Medical Eye AI system and two ophthalmologists (retina experts, Kappa(κ)=0.844, 0.864). The sensitivity and specificity of AI automatic staging were evaluated based on the results of ophthalmologists’ staging.
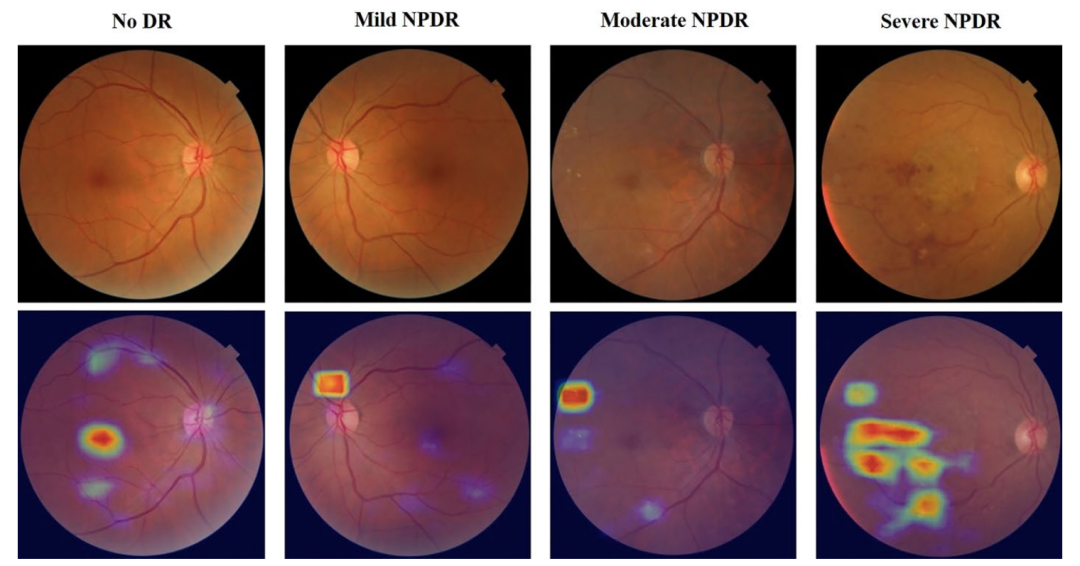
Exudation (white border box) and cystoid macular edema (purple border box).
DME is the most common cause of visual loss in patients with diabetic retinopathy, with an incidence of 2.7%-11% in patients with diabetic retinopathy, depending on the type of diabetes and duration of the disease. However, for type 1 and type 2 diabetes, the incidence of DME is about 30% after 25 years.
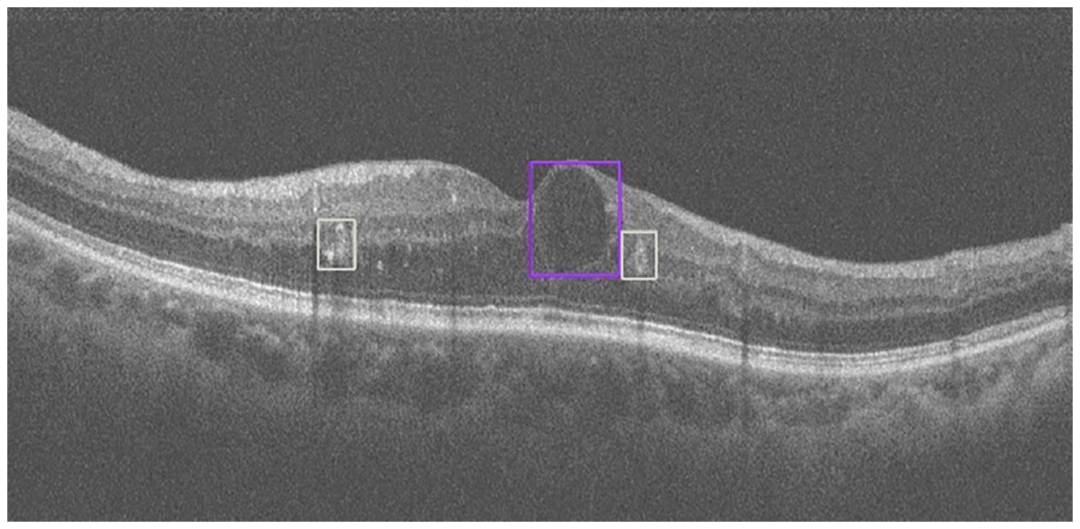
In DME, increased extracellular fluid from hyperpermeable retinal capillaries leads to macular thickening and affects central vision. It is worth noting that DME can occur at any stage of DR, whether it is non-proliferative diabetic retinopathy (NPDR) or proliferative diabetic retinopathy (PDR). However, before the use of OCT, clinical studies of macular edema detection in DME were performed using two-dimensional non-stereoscopic digital fundus photography. Without stereoscopic vision, fundus photography uses thickened substitute markers to identify DME, such as lipid or local color changes in the macula near the fovea. Due to the influence of pupil size and refraction media, screening for DME using non-stereoscopic fundus photography may have a high false positive rate. The following figure shows the AI analysis result of OCT fundus images, which demonstrates the superiority of multi-modal retinal disease AI system compared with single-modal fundus photography AI.
b. A preretinal membrane (yellow border box) was detected based on OCT AI.
c. No apparent abnormalities were found on the fundus color photograph.
Research results:
Of the 601 participants, 81 (13.5%) were detected with DR by ophthalmologists, while 94 (15.6%) were detected with DR by AI. Among them, 45 (7.5%) and 53 (8.8%) participants were diagnosed as requiring referral for DR by ophthalmologists and AI, respectively.
AI detection of DR had a sensitivity, specificity and AUC of 91.67%, 96.92%, and 0.944, respectively. The sensitivity, specificity, and AUC of AI detection for DR requiring referral were 97.78%, 98.38%, and 0.981, respectively. Among OCT images, 49 cases of macular edema (ME) were detected by ophthalmologists (8.2%), while 57 cases of ME were detected by AI (9.5%). The sensitivity, specificity, and AUC of AI for ME detection were 91.30%, 97.46%, and 0.944, respectively. When combining fundus color photographs and OCT images, the number of referrals determined by ophthalmologists increased from 45 to 75, while that of AI increased from 53 to 85.
Conclusion:
In this study, AI-assisted screening for DR and ME based on fundus color photographs and OCT images showed high sensitivity and specificity. This system can be implemented in community hospitals to identify more patients requiring referral and improve the referral rate for DR in the community.








No comments yet.